I will never forget a patient I saw leave the hospital on hospice care with grade 4 hepatitis following a single dose of immunotherapy. She spent the final weeks of her life in the hospital while we worked tirelessly to treat her side effects, and she eventually chose to go home after we had done all we could offer. Her story got me thinking: “Could we have given her a better quality of life by talking to her sooner about palliative care, or by getting her out of the hospital sooner with hospice services?” I wonder how often we delay integration of palliative care services since the advent of immunotherapy in oncology. How often do we treat immunotherapy as a “Hail Mary,” hoping that a final pass makes it into the end zone for the game-winning, life-saving touchdown? And as a pharmacist, what can I do to help my providers and patients make informed decisions that may affect quality of life, and prevent and relieve unnecessary suffering?
Immunotherapy and Palliative Care
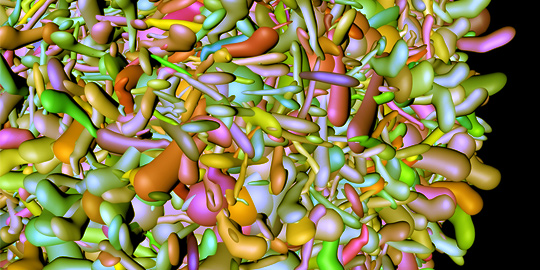
Immunotherapy has dramatically changed the management of several different solid tumors. Malignancies that previously had a poor prognosis now have hope of a durable response.1 Often believed to have a more favorable adverse event profile, immunotherapy is used at various points throughout treatment, first-line in some cases, and as a “Hail Mary” in others. And as we gain more experience with these drugs, more data emerge about their toxicity profiles and how severe they can be. Unfortunately, administration of immunotherapy at the end of life does not differ much from chemotherapy at the end of life, with more patients receiving immunotherapy during the last 30 days of life dying in the hospital rather than at home or in hospice care. A correlation has also seen between late palliative care referrals (within 3 months of death) and increased hospital admissions during the final 30 days of life.2
Recent findings from Yeh and colleagues demonstrated a decrease in hospital length of stay in patients receiving outpatient palliative care services, which adds to years of data proving a myriad of benefits of palliative care in oncology patients: improved quality of life and burden of symptoms, increased caregiver and patient satisfaction, and improved overall survival.3,4 With a growing body of evidence to support early palliative care, why isn’t it happening?
Barriers to Implementation of Palliative Care
Many barriers exist to integrating palliative care services earlier in the treatment course for oncology patients. Aside from common misunderstanding of terminology even among healthcare professionals, adequate manpower to deliver palliative care services is not in place to meet the existing demand, much less if all patients who would qualify for palliative care sought referrals.4
Enter: Pharmacists.
Pharmacist Roles for Integration of Palliative Care Services for Oncology Patients
The role of pharmacists in the use of immunotherapy and management of its side effects is vast and varied. Working to our advantage is our availability at multiple points along the continuum of care. We are present in clinics, inpatient floors, and infusion rooms and are available in-person, by telephone, or virtually.5 We are key links to the continuity of care of oncology patients.5 We are trusted, knowledgeable professionals with a depth of understanding of the medications used for pain, along with other cancer- and treatment-related symptoms and side effects, and are often involved from the time of diagnosis until a patient receives a final dose of cancer-directed therapy.5 Inevitably we will see patients progress through multiple lines of treatment and will potentially be involved in the palliation of their symptoms.
A recent scoping review noted several opportunities for pharmacists in palliative care oncology.6 These opportunities include:
- Pain assessment and management
- Patient education of pain management, side effects of opioids
- Interpretation and application of pharmacogenomic testing
- Medication reconciliation at transitions of care
- Deprescribing
- Interventions for other symptoms, including fatigue, anxiety/depression, gastrointestinal toxicities (i.e., nausea, diarrhea), dyspnea, anorexia, and cachexia
And let’s not forget our unique training in drug information and literature interpretation. With our expertise in analyzing primary literature, we can review outcomes with our physician colleagues to ensure patients know what they can expect based on published scientific information when presented with different therapeutic options for their cancer treatment.
Consider a novel approach published by a group of oncology clinical pharmacists at Michigan Medicine.5 This group established a collaborative drug therapy management (CDTM) program that received referrals from physicians in adult hematology and oncology clinics for management of gastrointestinal toxicities. Patients were referred for nausea, vomiting, constipation, or diarrhea, and pharmacists had prescriptive authority under the CDTM agreement. Fifty-two patients were seen by pharmacists within the time frame of the study and had an average of 2.2 visits. Pharmacists educated patients on use of medications related to the above toxicities, recommended additional medications, and changed how patients should take medications. Over two-thirds of patients had improvement in symptom severity, and notably, only 3.8% of patients visited an emergency department for symptoms related to the referring diagnosis. These findings reveal an innovative framework for pharmacists to consider for patients in need of symptom management, and would provide an avenue for establishing early palliative care with oncology patients. Simultaneously, using pharmacists for medication optimization may decrease healthcare utilization in a pandemic-strained healthcare system.
What if we are the key?
Pharmacist services related to palliative care in oncology patients is an area for expansion of our clinical practice as the use of immunotherapy becomes more widespread and its side effects become long-lasting. While pharmacists with training in palliative care can provide these services, pharmacists working along other points of the continuum of care – inpatient, ambulatory clinic, specialty clinic – can also deliver these services to patients in collaboration with interdisciplinary team members. Consider the possibility of these services becoming revenue-generating,5 or using the framework referenced above to target specific symptoms based on the needs of your organization that can result in decreased healthcare utilization.5 What if we are the key to integrating early palliative care for oncology patients?
More Information
References
- Sanderson CR, Currow DC. Palliative care meets immunotherapy: what happens as cancer paradigms change? BMJ Support Palliat Care 2018;8:431-432. doi:10.1136/bmjspcare-2018-001598
- O’Sullivan HM, Conroy M, Power DG, et al. Immune checkpoint inhibitors and palliative care at the end of life: an Irish multicentre retrospective study. J Palliat Care doi: 10.1177/08258597221078391
- Yeh JC, Urman AR, Besaw RJ, et al. Different associations between inpatient or outpatient palliative care and end-of-life outcomes for hospitalized patients with cancer. JCO Oncol Pract 2022;18(4):e516-e524. doi: 10.1200/OP.21.00546
- Kayastha N, LeBlanc TW. Why are we failing to do what works? Musings on outpatient palliative care integration in cancer care. JCO Oncol Pract 2022;18(4):255-257. doi: 10/1200/OP.21.00794
- Homan MJ, Reid JH, Nachar VR, et al. Implementation and outcomes of a pharmacist-led collaborative drug therapy management program for oncology symptom management. Support Care Cancer 2021;29:6505-6510. doi: 10.1007/s00520-021-06239-0
- Franco J, de Souza RN, de M Lima T, et al. Role of clinical pharmacist in the palliative care of adults and elderly patients with cancer: a scoping review. J Oncol Pharm Practice 2022;28(3):664-685. doi: 10.1177/10781552211073470